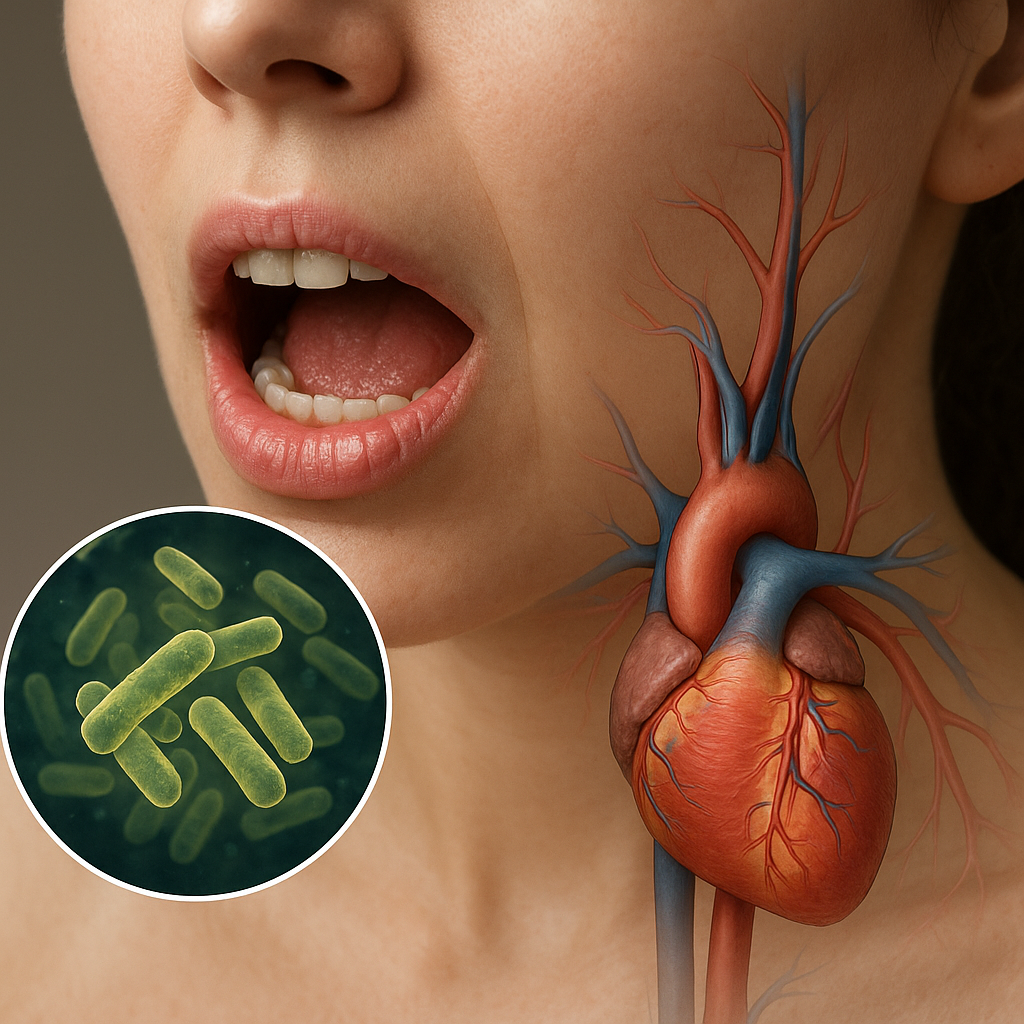
The intricate relationship between the oral environment and overall health has captured the attention of both researchers and practitioners. Understanding how oral bacteria contribute to systemic conditions is critical for dentists who strive to promote comprehensive well-being. This article explores the complex interplay between the oral microbiome and diseases beyond the mouth, outlining underlying mechanisms, associated health concerns, and practical steps clinicians can take to mitigate risk.
Understanding the Oral Microbiome
The human mouth hosts a vast ecosystem of microorganisms collectively known as the microbiome. This dynamic community includes hundreds of bacterial species organized into a structured biofilm that coats tooth surfaces and soft tissues. In health, beneficial bacteria like Streptococcus sanguinis and Actinomyces viscosus contribute to normal oral functions by preventing colonization of harmful pathogens and aiding in nutrient metabolism.
Disruption of this ecological balance—often due to poor hygiene, dietary sugars, or smoking—can lead to an overgrowth of pathogenic species such as Porphyromonas gingivalis and Fusobacterium nucleatum. These organisms release harmful enzymes and toxins, notably lipopolysaccharides (LPS), which trigger local inflammation. Persistent inflammation promotes gingival tissue destruction, pocket formation, and eventually periodontitis.
- Homeostasis: the state of microbial equilibrium supporting oral health
- Dysbiosis: microbial imbalance favoring disease-causing bacteria
- Biofilm maturation: a multi-step process involving adhesion, accumulation, and detachment
Maintaining a balanced oral ecology is essential not only for preventing cavities and gum disease but also for averting far-reaching systemic effects.
Pathogenic Mechanisms Linking Oral Bacteria to Systemic Disease
Oral pathogens can influence distant organs through several interrelated pathways. First, invasive bacteria breach the gingival barrier and enter the bloodstream, a phenomenon known as bacterial translocation. Routine activities such as brushing or chewing can induce transient bacteremia, allowing microbes to disseminate throughout the body.
Second, sustained oral infection elevates circulating pro-inflammatory mediators. Periodontal lesions produce cytokines like interleukin-6 and tumor necrosis factor-alpha, which amplify systemic inflammation and may destabilize atherosclerotic plaques in arteries.
Third, secreted bacterial products—including LPS and proteases—exert toxic effects on remote tissues. For example, gingipains from P. gingivalis degrade host proteins, impair immune defenses, and facilitate colonization in sites such as the arterial walls or the placenta.
Immune Response and Molecular Mimicry
Some oral bacteria exhibit antigens resembling host molecules. This immune cross-reactivity can induce autoantibody production, contributing to conditions like rheumatoid arthritis. Clinicians observing unexplained joint pain in periodontitis patients should consider interdisciplinary referrals.
Endothelial Dysfunction
Chronic exposure to oral pathogens promotes endothelial cell activation, characterized by upregulated adhesion molecules and increased vascular permeability. This process underlies the link between gum disease and cardiovascular disorders.
Systemic Conditions Associated with Oral Bacteria
Evidence supports associations between periodontal infection and multiple chronic illnesses. While causality remains under investigation, managing oral disease is prudent for reducing potential systemic burden.
Cardiovascular Disease
Patients with periodontitis exhibit higher rates of coronary artery disease, stroke, and peripheral vascular disease. P. gingivalis DNA has been detected within atherosclerotic plaques, suggesting direct bacterial involvement. Additionally, elevated C-reactive protein levels in periodontitis patients indicate systemic inflammation contributing to plaque instability.
Diabetes Mellitus
Diabetes and periodontal disease share a bidirectional relationship. Uncontrolled blood sugar fosters a hyperinflammatory response to oral bacteria, worsening tissue breakdown. Conversely, severe periodontitis impairs glycemic control by elevating insulin resistance. Improved periodontal therapy often corresponds with modest reductions in glycated hemoglobin (HbA1c).
Respiratory Infections
Aspiration of oral pathogens can seed the lower respiratory tract, leading to pneumonia in hospitalized or elderly individuals. Regular oral hygiene and professional dental care are proven strategies to decrease ventilator-associated pneumonia in critical care settings.
Adverse Pregnancy Outcomes
Pregnant women with untreated periodontitis face higher risk of preterm birth and low birth weight infants. Oral bacteria may translocate to the amniotic fluid, provoking premature labor through inflammatory cascades. Dental evaluation and appropriate periodontal treatment before or during pregnancy can mitigate these risks.
Clinical Implications for Dental Practice
Recognizing the systemic impact of oral infections transforms the role of dentists from focusing solely on teeth to safeguarding overall health. Incorporating medical screening and patient education into routine care strengthens preventive efforts.
Risk Assessment and Screening
Implement comprehensive medical histories that include cardiovascular, diabetic, and obstetric status. Monitor periodontal indices—probing depth, clinical attachment loss, and bleeding on probing—to stratify patient risk for systemic complications.
Preventive Strategies
- Emphasize twice-daily brushing with fluoridated toothpaste and interdental cleaning
- Recommend antimicrobial mouth rinses when indicated
- Advise smoking cessation to restore microbial equilibrium
- Coordinate with physicians to optimize management of chronic diseases
Patient motivation and self-care are vital. Empower individuals through clear guidance on plaque control and lifestyle modifications.
Interprofessional Collaboration
Effective communication between dentists, physicians, and specialists enhances patient outcomes. Sharing diagnostic findings and treatment plans fosters a unified approach to managing systemic risk factors. Referral networks ensure timely interventions for high-risk individuals.
Emerging Research and Future Directions
Ongoing studies explore novel therapeutic targets within the oral microbiome. Probiotic formulations aim to restore healthy microbial communities and suppress pathogenic overgrowth. Vaccine research against key periodontal pathogens represents a promising frontier. Advances in salivary diagnostics could enable early detection of systemic disease markers before clinical onset.
Personalized medicine—leveraging genetic and microbiome profiling—may soon guide individualized preventive and treatment plans. By integrating cutting-edge technologies and fostering interdisciplinary partnerships, the dental profession stands poised to impact not only oral health but the entire human body.